Have you experienced a hot flush, a panic attack, insomnia or a change in menstrual flow and been unable to pinpoint the exact cause? These symptoms—and many others—can be early signs of perimenopause.
While the perimenopause is most likely to start in a woman’s 40s, for some it can begin as early as her 30s, or even earlier in the case of a surgical menopause (a total or radical hysterectomy where the ovaries are removed). And this transitional time can last anywhere from two to 12 years.
Recognising this important life stage early presents you with greater opportunities to invest in your health, build a strong foundation and manage any troublesome symptoms. Here are five tips to help you navigate perimenopause and make it a positive and empowering journey.
1. Knowledge is power
Menopause marks the one year anniversary of your last menstrual period, whereas perimenopause is the time period prior to this when you’ll have cycles, but start to experience menopausal symptoms. It is characterised by incremental changes in female hormones, namely oestrogen and progesterone. For some women these changes can be very subtle, but for others this period can be significant and have a huge impact on quality of life. Due to the hormonal shift a wide range of symptoms can appear and they can evolve and change in subsequent years.
Typically, in the early stages of perimenopause, oestrogen levels are relatively high compared to progesterone and this can cause heavier periods and also shorter menstrual cycles. Symptoms such as breast tenderness, headaches, night sweats, insomnia, anxiety and hot flashes can dominate. Towards the later stages of perimenopause, as women approach menopause, oestrogen declines and periods will become less frequent and unpredictable. Different symptoms may start to occur such as bladder urgency and frequency, painful sex, and joint and muscle pain.
Management of these symptoms can be as simple as addressing lifestyle factors such as sleep, nutrition and stress management. Further treatment may include topical oestrogen or menopausal hormone therapy, which is best known as hormone replacement therapy (HRT). While, historically, HRT has courted controversy, doing your own research, talking to your GP and finding what works for you is the most important message. Everyone's experience of this transition will be unique, however, understanding the process will enable you to be proactive and reach out for help when necessary.
2. Track your period and symptoms
The best way to recognise the signs of perimenopause is to track your period and work out what is “normal” for you so you can then identify changes in your period or accompanying symptoms, their severity and impact on your daily life. Your period can change over the years, and as you get older typically your cycle gets shorter and increasingly irregular. Cycle tracking should include information such as length, flow and symptoms including pain, cramping, mood, sleep and gastrointestinal changes. There are plenty of apps that can assist with tracking, including Clue, Eve, Flo and Spot On. If you have further concerns about your menstrual cycle, seeking medical support is recommended.
3. Keep moving
Exercise during the perimenopausal life stage is non-negotiable and its benefits are well researched. It has a positive influence on so many different body systems, including the cardiovascular, mental, digestive and musculoskeletal.
Did you know that one in three women over the age of 50 will experience a fracture due to osteoporosis? Exercise is crucial to maintaining good bone health in your perimenopausal years and builds a solid foundation for the future. From your 40s, you begin to lose more bone than you make and this process continues at pace until the menopause. The good news is, it’s never too late to take action, as your bones are constantly changing and will respond to stress and load. This is why high-impact activities such as jogging, tennis, dancing or simply stomping up the stairs builds healthy bones. Strength training, body weight exercises such as planks, squats, lunges and resistance band exercise should also be a priority as they help to maintain muscle mass and body strength, both of which decline with a reduction in oestrogen. Movement is also essential to supporting regular bowel function and in turn a healthy pelvic floor system.
4. Address any pelvic health issues
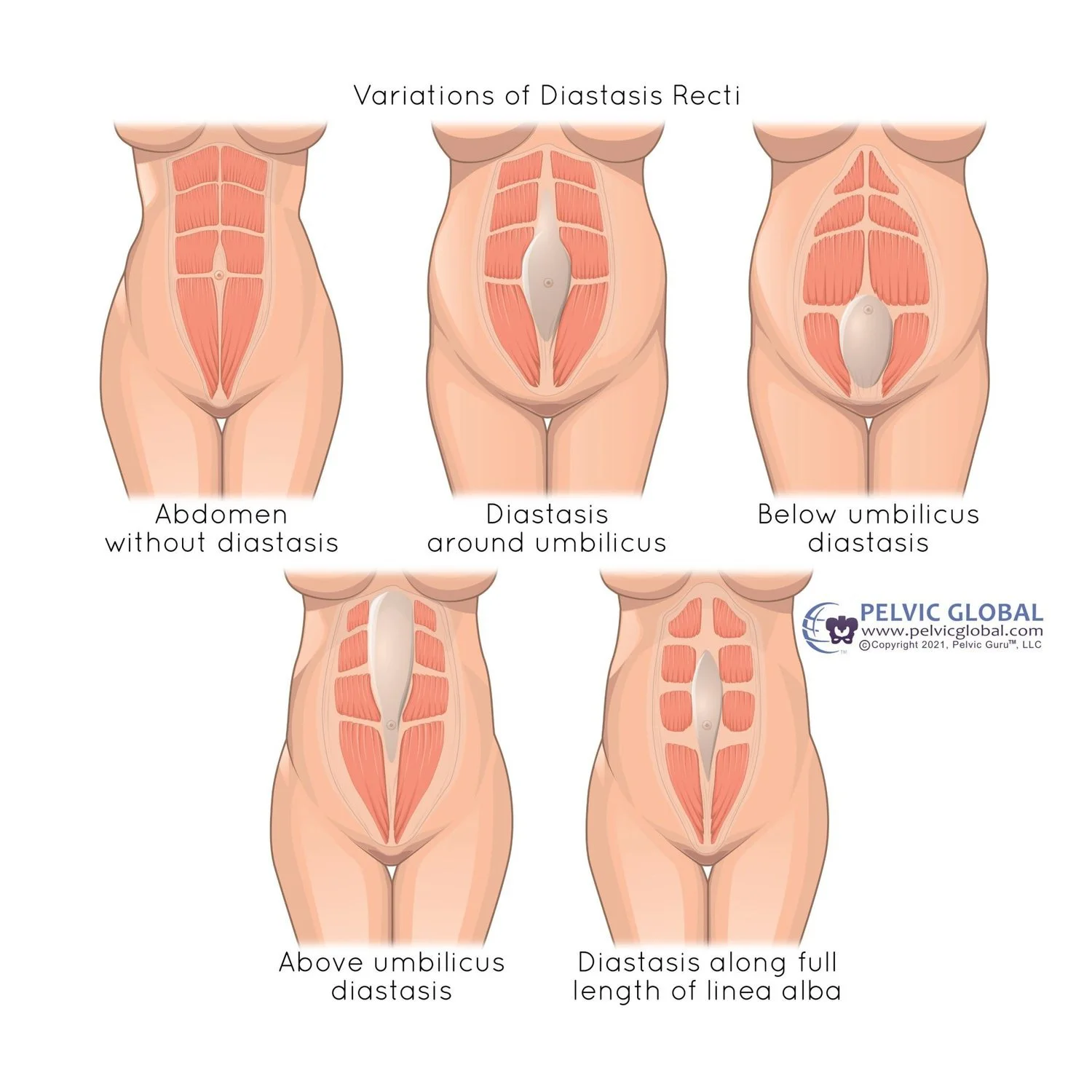
Don’t let pelvic floor symptoms become a roadblock to exercise or life quality. A significant number of women—upwards of 54 percent—suffer symptoms such as painful sex, urinary or anal incontinence, and urinary frequency—and accept them as a normal part of ageing without seeking medical help. The decline in oestrogen in perimenopause can lead to changes in the genito-urinary system, but there are plenty of things you can do. A good starting point is a women’s health physiotherapist for specific assessment and treatment of any pelvic floor issues. Research supports pelvic floor muscle strength re-training programmes, which can help to treat stress incontinence. Individualised help can also address many less-talked-about issues such as painful sex, vaginal dryness and flatus. Some quick fixes may be as easy as using a vaginal lubricant, pelvis and/or hip stretches or changing sexual positions.
5. Ride the wave
Feeling moody, anxious or irritable are some of the more commonly reported emotional experiences associated with perimenopause. Accepting that these feelings may occasionally surface and be part of your perimenopause journey is the first step. It may also be worth considering whether some of these things need a closer look. Are you always getting irritated by the same thing? Perhaps it’s the situation you’re in that needs changing. Have you always felt a bit anxious, but now it’s worse? Try learning some anxiety management strategies. Keep track of your moodiness and other emotions in the same way you would your cycle. This can help you to recognise, accept and ride the wave. If you need time for yourself, take it. Stop putting everyone else first.
It’s worth remembering that perimenopause and menopause are natural processes that our bodies are designed to go through. Consider the other things our bodies are designed to do: to move—all the time. Where are our stress levels designed to be? Low—only triggered by an actual threat to our physical safety. What diet is our body designed to need? Fresh produce, whole foods, nothing artificial. How are we designed to breathe? Slowly, deeply, fully. We’re meant to connect with nature—trees and soil release microorganisms that are beneficial to human health. The more you can get back into balance with the things that your body is designed to do, the more you can ride the wave of perimenopause with less anxiety and resistance.
Kathryn Gale is a registered psychologist and mindfulness meditation coach at Joint Dynamics Evolve.
Kym Toller is a women’s health physiotherapist at Joint Dynamics Evolve.